Researchers initiated 7,584 cancer biopsies from 16 different cancer types. Each biopsy was sliced into thin sections and prepared using a method known as standard hematoxylin and eosin staining to visualize the overall appearance of cancer cells. Information about the cancer’s transcriptome (which genes are actively used by cells) was also available.
practical model
After the researchers integrated the new cancer biopsies with other datasets, including transcriptome data and images from thousands of healthy cells, they used SEQUOIA (a slide-based An AI program named Expression Quantification) was able to predict expression. Extract patterns for over 15,000 different genes from stained images. For some cancer types, AI-predicted gene activity correlated more than 80% with actual gene activity data. In general, the more samples of a particular cancer type that are included in the initial data, the better the model will perform for that cancer type.
“We had to iterate the model many times before we reached satisfactory performance,” says Gevaert. “But eventually, for some tumor types, we reached a point where it would be useful in the clinic.”
Professor Gewald pointed out that rather than looking at one gene at a time to make clinical decisions, doctors often look at genetic signatures that include hundreds of different genes. For example, many cancer cells activate the same group of hundreds of genes associated with inflammation, or hundreds of genes associated with cell proliferation. Compared to its performance in predicting individual gene expression, SEQUOIA was even more accurate in predicting whether such large-scale genomic programs were activated.
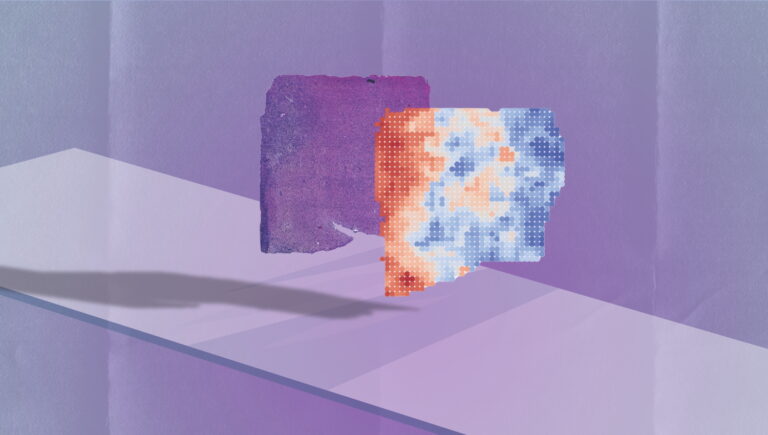
To make data easier to access and interpret, the researchers programmed SEQUOIA to display genetic findings as a visual map of tumor biopsies, allowing scientists and clinicians to visualize genetic findings in different regions of the tumor. We made it possible to see how the target mutations differ.
Predict patient outcomes
To test the utility of SEQUOIA in clinical decision-making, Gevaert and colleagues identified breast cancer genes whose expression the model could accurately predict and were already used in commercial breast cancer genomic tests. (For example, the Food and Drug Administration-approved MammaPrint test analyzes levels of 70 breast cancer-related genes to provide patients with a score of how likely their cancer is to come back.)
“Breast cancer has a number of well-studied genetic signatures that have been shown over the past decade to be highly correlated with treatment response and patient outcomes,” Gevaert said. said. “This made this an ideal test case for our model.”
The research team showed that SEQUOIA can provide the same type of genomic risk score as MammaPrint using only stained images of tumor biopsies. This result was repeated in multiple different groups of breast cancer patients. In both cases, patients identified as high risk by SEQUOIA had worse outcomes, with higher rates of cancer recurrence and shorter time to cancer recurrence.
AI models cannot yet be used in clinical practice. It must be tested in clinical trials and approved by the FDA before it can be used to guide treatment decisions. But Gewald said his team is refining the algorithm and studying its potential applications. . In the future, SEQUOIA could reduce the need for expensive gene expression tests, he said.
“We showed how this helps in breast cancer, and now we can use it in all cancers to characterize every gene that’s there,” he said. Ta. “This is a completely new data source that has never existed before.”
Scientists from Roche Diagnostics were also authors of the paper.
Funding for this research was provided by the National Cancer Institute (grant R01 CA260271), a Belgian American Educational Foundation Fellowship, the Wetenschappelijk Onderzoek-Vlaanderen Foundation, the Fulbright Spanish Commission, and a grant from Ghent University. I did.